Friday, 25 September 2009
Thursday, 24 September 2009
The Physiology of Depression
The physiology of mood disorders is complicated, and not particularly well understood. What we do know comes from brain imaging and looking at the levels of different chemicals in the brain. There may be some long, confusing words you've never heard of here, but stick with it, because what this stuff tells us is important.
In unipolar depression, the physical problem is believed to be an imbalance of either serotonin, noradrenaline or dopamine in the brain; or two or all three of those. Exactly how we don't know, and the exact imbalance is probably different for everybody, but generally speaking, most people with depression have less serotonin, or noradrenaline in their brain than healthy people do. The pathophysiology of Bipolar Disorder is poorly understood, but it is probably linked to the same three neurotransmitters as well as some structural abnormalities in the amygdala, basal ganglia and prefrontal cortex.1
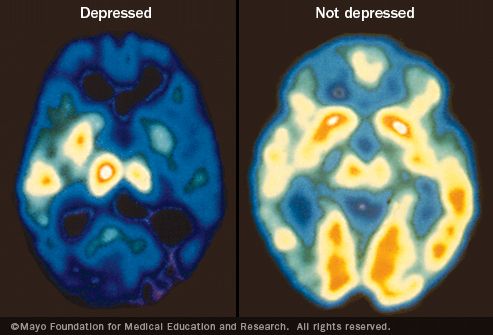
PET (Positron Emission Topography) and SPECT (Single Proton Emission Computed Topography) scans are two types of brain scans which show how active or inactive the different areas of the brain are. PET scans of depressed brains compared to normal ones show a significant reduction in overall brain activity. This is why everything seems ten times harder when you're depressed and why it's much harder to concentrate and remember things. People with depression are like cars running on half a tank of gas, or in some cases hardly any gas at all. You can barely get out of the driveway, let alone make it around the block. In other words, if you're depressed, you can't expect yourself to carry on with your normal life while you are ill. So give yourself a break!
In people with Bipolar Disorder, PET and SPECT imaging usually shows decreased activity in the prefrontal cortex, which is involved in emotion and planning, the amygdala, which is associated with mood regulation, and the hippocampus2. This may explain the intense highs and lows bipolar sufferers experience. Patients in the depressed phased of a cycle show very similar scan results to patients with unipolar depression. In the manic phase, imaging shows both left-right and dorso-ventral asymmetry in the basal temporal cortex. I have absolutely no idea what that means.
But whether you have any idea of what a basal temporal cortex is or not, the important thing to understand is that...
Sources:
1. Internet Mental Health
2. Rachel Pollock, PhD & Irving Kuo, MD - "Neuroimaging in Bipolar Disorder"
3. Jerod Poore, Crazy Meds
4. Karl Hempel, MD - "Depression: What You Need To Know"
5. Amen Clinics SPECT Imaging
In unipolar depression, the physical problem is believed to be an imbalance of either serotonin, noradrenaline or dopamine in the brain; or two or all three of those. Exactly how we don't know, and the exact imbalance is probably different for everybody, but generally speaking, most people with depression have less serotonin, or noradrenaline in their brain than healthy people do. The pathophysiology of Bipolar Disorder is poorly understood, but it is probably linked to the same three neurotransmitters as well as some structural abnormalities in the amygdala, basal ganglia and prefrontal cortex.1
PET (Positron Emission Topography) and SPECT (Single Proton Emission Computed Topography) scans are two types of brain scans which show how active or inactive the different areas of the brain are. PET scans of depressed brains compared to normal ones show a significant reduction in overall brain activity. This is why everything seems ten times harder when you're depressed and why it's much harder to concentrate and remember things. People with depression are like cars running on half a tank of gas, or in some cases hardly any gas at all. You can barely get out of the driveway, let alone make it around the block. In other words, if you're depressed, you can't expect yourself to carry on with your normal life while you are ill. So give yourself a break!
In people with Bipolar Disorder, PET and SPECT imaging usually shows decreased activity in the prefrontal cortex, which is involved in emotion and planning, the amygdala, which is associated with mood regulation, and the hippocampus2. This may explain the intense highs and lows bipolar sufferers experience. Patients in the depressed phased of a cycle show very similar scan results to patients with unipolar depression. In the manic phase, imaging shows both left-right and dorso-ventral asymmetry in the basal temporal cortex. I have absolutely no idea what that means.
But whether you have any idea of what a basal temporal cortex is or not, the important thing to understand is that...
[in serious mental illness] Your brain is physically injured, and like any other part of the body that has received a physical injury, it needs the proper care to heal... The problem that far too many people have is that they can't see the injury, therefore it is not a real injury... - Jerod Poore, Crazy Meds 3Whether you suffer from a mood disorder or not, you should know that they are genuine medical conditions with physical manifestations in the brain. Just because you can't see the physical problem, it doesn't mean that it's not there. If you could have one of those fancy brain scans yourself, you would see it. Use this information to accept the fact that you're ill, and you need rest and medical treatment. You're not weak or selfish or any of the other things people may accuse you of. You're not well. Got it? Good.
Sources:
1. Internet Mental Health
2. Rachel Pollock, PhD & Irving Kuo, MD - "Neuroimaging in Bipolar Disorder"
3. Jerod Poore, Crazy Meds
4. Karl Hempel, MD - "Depression: What You Need To Know"
5. Amen Clinics SPECT Imaging
Monday, 21 September 2009
Other Types of Depression
So if you read the first on depression, you know what clinical depression is, the symptoms and some of the possible causes. But there are other types of unipolar depression too.
Dysthymia
Dysthymia (or Dysthymic Disorder) is a form of depression which is less severe than major depression, but which is chronic and persistant. People are diagnosed with Dysthymia if they have felt depressed more than half of the time for at least two years, but their depressed mood is either not severe enough to justify a diagnosis of clinical depression or it only occurs in shorter episodes. However, it's common for Dysthymia to lead to a diagnosis of clinical depression: 75% of people with Dysthymia will go on to develop clinical depression within 5 years of being diagnosed.
The diagnostic criteria are as follows:
A. Depressed mood more than half the time for at least 2 years.
B. When depressed, two or more of the following symptoms are present:
(1) Appetite increased or decreased
(2) Sleep increased or decreased
(3) Fatigue
(4) Poor self-image
(5) Attachment to relatives other than parents
(6) Concentration and decisiveness decreased
(7) Feelings of hopelessness or pessimism.
C. During the 2-year period, symptoms were not absent for 2 months or longer.
D. During first 2 years, the patient has not had a Major Depressive Episode
E. Patient has never had a manic, hypomanic or mixed state.
F. Patient has never met the criteria for Cyclothymia
Seasonal Affective Disorder
Seasonal Affective Disorder (SAD) is a condition which is characterised by normal mental health most of the year, with symptoms of depression only occuring during the winter months. The symptoms normally begin in September and get worse as the winter progresses, starting to go away in early spring. Up to eight in 10 people experience some tiredness, increased appetite or anxiety in the winter months because of the low levels of bright light. When light enters the eye, it stimulates nerve impulses to travel to the hypothalamus - the part of the brain which controls mood, appetite, sleep, temperature and sex drive. So when light levels decrease in the winter, all of those things are affected.
Light therapy has been shown to be effective in up to 85 per cent of diagnosed cases of seasonal affective disorder. It involves sitting in front of a special lamp or light box which is about ten times brighter than normal household lighting. In mild cases just making the effort to spend time outside in the daylight may be of benefit. In severe cases, antidepressants may be used, but this is not ideal because they can make some of the symptom, like sleep problems, worse rather than better.
In some rare cases people experience a form of SAD in the summer months. The symptoms of Summer SAD are pretty much the opposite, including insomnia, weight loss, agitation, reduced appetite, irritability and increased sex drive.
Postnatal Depression
Also known as Postpartum Depression (PPD). PND is a type of depression which affects many women after they give birth. It can start at any time within a year of the birth, but it most commonly starts in the first 4-6 weeks. As many as one in ten new mothers experience PND, often without recognising it, and the longer the illness goes untreated, the longer it's likely to last. PND is a temporary and very treatable condition.
If you have any of the following warning signs, it's vital that you seek medical attention as soon as possible, or report your feelings to your health visitor.
It's now becoming recognised that fathers can also suffer from depression after the arrival of a new baby, especially if the mother is suffering from PND. Having a new baby brings lots of stressful changes, like increased responsibility, worrying about the cost of raising a child, changes in the relationship between the parents, having more stress and jobs to do at home as well as not having as much sleep. Men sometimes feel hostile and angry when they are depressed, and this can lead to guilt, plus home visitors or health workers might be critical of them or see them as potentially violent. Again, symptoms should be discussed with a doctor as soon as possible to prevent harm to the child or to the relationship between father and mother.
Sources:
The Mental Health Foundation
MIND
Internet Mental Health
Dysthymia
Dysthymia (or Dysthymic Disorder) is a form of depression which is less severe than major depression, but which is chronic and persistant. People are diagnosed with Dysthymia if they have felt depressed more than half of the time for at least two years, but their depressed mood is either not severe enough to justify a diagnosis of clinical depression or it only occurs in shorter episodes. However, it's common for Dysthymia to lead to a diagnosis of clinical depression: 75% of people with Dysthymia will go on to develop clinical depression within 5 years of being diagnosed.
The diagnostic criteria are as follows:
A. Depressed mood more than half the time for at least 2 years.
B. When depressed, two or more of the following symptoms are present:
(1) Appetite increased or decreased
(2) Sleep increased or decreased
(3) Fatigue
(4) Poor self-image
(5) Attachment to relatives other than parents
(6) Concentration and decisiveness decreased
(7) Feelings of hopelessness or pessimism.
C. During the 2-year period, symptoms were not absent for 2 months or longer.
D. During first 2 years, the patient has not had a Major Depressive Episode
E. Patient has never had a manic, hypomanic or mixed state.
F. Patient has never met the criteria for Cyclothymia
Seasonal Affective Disorder
Seasonal Affective Disorder (SAD) is a condition which is characterised by normal mental health most of the year, with symptoms of depression only occuring during the winter months. The symptoms normally begin in September and get worse as the winter progresses, starting to go away in early spring. Up to eight in 10 people experience some tiredness, increased appetite or anxiety in the winter months because of the low levels of bright light. When light enters the eye, it stimulates nerve impulses to travel to the hypothalamus - the part of the brain which controls mood, appetite, sleep, temperature and sex drive. So when light levels decrease in the winter, all of those things are affected.
Light therapy has been shown to be effective in up to 85 per cent of diagnosed cases of seasonal affective disorder. It involves sitting in front of a special lamp or light box which is about ten times brighter than normal household lighting. In mild cases just making the effort to spend time outside in the daylight may be of benefit. In severe cases, antidepressants may be used, but this is not ideal because they can make some of the symptom, like sleep problems, worse rather than better.
In some rare cases people experience a form of SAD in the summer months. The symptoms of Summer SAD are pretty much the opposite, including insomnia, weight loss, agitation, reduced appetite, irritability and increased sex drive.
Postnatal Depression
Also known as Postpartum Depression (PPD). PND is a type of depression which affects many women after they give birth. It can start at any time within a year of the birth, but it most commonly starts in the first 4-6 weeks. As many as one in ten new mothers experience PND, often without recognising it, and the longer the illness goes untreated, the longer it's likely to last. PND is a temporary and very treatable condition.
If you have any of the following warning signs, it's vital that you seek medical attention as soon as possible, or report your feelings to your health visitor.
- Feeling very sad or low, crying a lot.
- Feeling very tired, or 'numb' and not wanting to do anything or not having interest in the baby.
- Feeling hopeless and like you can't cope, and feeling very guilty as a result.
- Feeling like you're not attached to your baby, or thinking that you're a bad mother because you don't love your baby enough.
- Being unusually irritable, which may make you feel even more guilty.
- Having problems sleeping
- Losing your appetite
- Losing interest in sex
- Being hostile or indifferent to your partner or your baby
- Feeling very anxious, worrying constantly about the baby or your own health, or having panic attacks
- Feeling unable to concentrate or finding normal tasks overwhelming
- Thoughts about death or suicide
It's now becoming recognised that fathers can also suffer from depression after the arrival of a new baby, especially if the mother is suffering from PND. Having a new baby brings lots of stressful changes, like increased responsibility, worrying about the cost of raising a child, changes in the relationship between the parents, having more stress and jobs to do at home as well as not having as much sleep. Men sometimes feel hostile and angry when they are depressed, and this can lead to guilt, plus home visitors or health workers might be critical of them or see them as potentially violent. Again, symptoms should be discussed with a doctor as soon as possible to prevent harm to the child or to the relationship between father and mother.
Sources:
The Mental Health Foundation
MIND
Internet Mental Health
Saturday, 19 September 2009
Bipolar Depression
Bipolar Depression is a kind of mood disorder which causes periods of low or depressed mood like those which people with unipolar depression experience, but people with bipolar depression also have periods of elevated mood, which can be either 'mania' or 'hypomania'. It's also known as Manic Depression or Bipolar Disorder.
Somebody who is having a manic episode usually feels elated or euphoric, but it can also make people irritable. They may be easily distracted, have a low attention span, increased sex drive, unusual impulsive behaviour and racing thoughts. Sometimes a person can become aggressive, feel unstoppable, or have delusional ideas such as that they are "chosen" or "on a special mission". At its most severe, manic symptoms can progress to full-blown psychosis.
Hypomania is a shorter and less extreme version of mania, still with elevated or irritable mood but with fewer symptoms and less severity. A 'mixed episode' is one where symptoms of depression and mania are present at the same time.
There are three specific types of Bipolar Disorder - Bipolar I, Bipolar II and Cyclothymia. Some people, however, may have an illness which seems to be a kind of bipolar depression but they don't fit into any of the three categories. Those people might be technically labelled with 'Bipolar Disorder Not Otherwise Specified'.
Bipolar I Disorder
It's also poorly treated. Only around 5 per cent have psychological therapy and just a third of known sufferers have a yearly check of their state of mind.3 Many famously creative individuals are known or believed to have suffered from bipolar disorder, e.g. Vincent Van Gough, Spike Milligan, Sylvia Plath, Virginia Woolf, and Ernest Hemingway. Stephen Fry, a much-loved British actor and comedian, is one such example. He has openly admitted to having manic depression - specifically cyclothymia.4 He famously walked out on a part in a West End show called Cell Mates and disappeared. It later emerged that he had tried to kill himself, then took a ferry to France and eventually went to America for treatment. Of his own diagnosis, he said, and I quote:
Bipolar disorder has the highest suicide rate of any psychiatric illness. Around 15% of sufferers kill themselves. This makes the shockingly low rate of diagnosis and proper care for those with the illness all the more worrying. For more information, try the following resources:
Sources:
1, 2, 3. The Independent, "Stephen Fry: My Battle With Mental Illness"
4. BBC "The Secret Life Of Depression" microsite
5. Stephen Fry - "The Secret Life Of Depression"
Somebody who is having a manic episode usually feels elated or euphoric, but it can also make people irritable. They may be easily distracted, have a low attention span, increased sex drive, unusual impulsive behaviour and racing thoughts. Sometimes a person can become aggressive, feel unstoppable, or have delusional ideas such as that they are "chosen" or "on a special mission". At its most severe, manic symptoms can progress to full-blown psychosis.
Hypomania is a shorter and less extreme version of mania, still with elevated or irritable mood but with fewer symptoms and less severity. A 'mixed episode' is one where symptoms of depression and mania are present at the same time.
There are three specific types of Bipolar Disorder - Bipolar I, Bipolar II and Cyclothymia. Some people, however, may have an illness which seems to be a kind of bipolar depression but they don't fit into any of the three categories. Those people might be technically labelled with 'Bipolar Disorder Not Otherwise Specified'.
Bipolar I Disorder
- People with Bipolar I will have had at least one full manic episode.
- A diagnosis of Bipolar I requires only the presence of one manic episode, but many people with Bipolar I experience periods of major depression or hypomania as well.
- Bipolar I is the most severe form of Bipolar Depression.
- Bipolar II is characterised by cycles of depressed episodes and hypomanic episodes.
- To be diagnosed with Bipolar II, the sufferer has to have had at least one hypomanic episode, and at least one major depressive episode.
- Only people who have never had a manic episode are diagnosed with Bipolar II. If somebody with Bipolar II experiences a manic episode, their diagnosis will be changed to Bipolar I.
- Cyclothymia is a chronic type of Bipolar Depression where hypomanic episodes are present chronically for at least 2 years, but without any periods of clinical depression
- People with Cyclothymia can experience chronic low mood, but not severe enough to quality as a major depressive episode, so they do not fulfull the criteria for a diagnosis of Bipolar II.
- The longest period somebdoy with cyclothymia has been free of symptoms is two months. If it's more than that, they will be given a different diagnosis.
"Bipolar has the highest suicide rate out of all mental illnesses... So people not treated soon enough are having their lives put at risk."2
"I'd never heard the word before, but for the first time, at the age of 37, I had a diagnosis that explains the massive highs and miserable lows I've lived with all my life ... There's no doubt that I do have extremes of mood that are greater than just about anybody else I know. The psychiatrist in the hospital recommended I take a long break... My mind was full of questions. Am I now mad? How have I got this illness, could it have been prevented, can I be cured of it? Since then, I have discovered just how serious it is to have bipolarity, or manic depression as it's also called. Four million others in the UK have it and many of them end up killing themselves."5
Bipolar disorder has the highest suicide rate of any psychiatric illness. Around 15% of sufferers kill themselves. This makes the shockingly low rate of diagnosis and proper care for those with the illness all the more worrying. For more information, try the following resources:
Sources:
1, 2, 3. The Independent, "Stephen Fry: My Battle With Mental Illness"
4. BBC "The Secret Life Of Depression" microsite
5. Stephen Fry - "The Secret Life Of Depression"
Friday, 18 September 2009
What Is Depression?
Depression is a mental illness which involves feelings of intense sadness, hopelessness and low self-esteem which won't go away, along with physical symptoms like sleeplessness, a loss of energy, or physical aches and pains. Depression is different from feeling low, even though people often say "I'm depressed" when they feel a bit down. Mild to moderate depression is common, and while it usually doesn't stop you from doing your normal daily activities, it does make everything harder to do and seem less worthwhile.
Severe depression is extremely distressing and makes normal activity near impossible. It can be life-threatening, since many people with severe depression attempt suicide. Somebody with severe depression might stay in bed for days or weeks on end because they don't have the energy to do anything else. This kind of depression gets you labelled with 'Major Depression' or 'Major Depressive Disorder'. It is also sometimes called 'unipolar' depression, to distinguish it from bipolar depression.
Symptoms
The most common symptoms of depression are:
Causes
The exact cause of depression is not known, but the likelihood that somebody will decome depressed seems to be determined by a combination of physical, psychological and social factors.
Some types of depression run in families, so it's thought that some people inherit a genetic predisposition for it. In identical twins, if one twin is diagnosed with clinical depression, the other twin has around a 46% chance of developing one too. Other people affected by depression have no family history of mental illness, but they may be vulnerable to depression because they have picked up very negative ways of thinking. Low self-esteem and distorted thinking are closely related to depression, although it's not always clear if they are a cause or an effect.
Depression can be triggered by a traumatic event or period of stress, such as a bereavement, losing a job, family problems, divorce, exam stress, poverty or social isolation. Substance abuse and certain chronic illnesses (e.g. hypothyroidism) also make people more likely to develop depression.
More about depression:
Sources:
1. The Depression Alliance - Now We're Talking (April 17, 2007)
2. NPR - History of Treating Depression (2004)
3. Karl Hempel, M.D. - Depression: What you need to know
Severe depression is extremely distressing and makes normal activity near impossible. It can be life-threatening, since many people with severe depression attempt suicide. Somebody with severe depression might stay in bed for days or weeks on end because they don't have the energy to do anything else. This kind of depression gets you labelled with 'Major Depression' or 'Major Depressive Disorder'. It is also sometimes called 'unipolar' depression, to distinguish it from bipolar depression.
Symptoms
The most common symptoms of depression are:
- Low mood, which varies little from day to day.
- Loss of interest, pleasure and concentration
- Loss of energy, tiredness even after little effort.
- Loss of appetite, or increased appetite
- Weight loss when not dieting or weight gain
- Insomnia & sleeplessness, or excessive sleepiness
- Visible agitation or slowed movements
- Feelings of worthlessness, low self-esteem, low self-confidence
- Excessive or inappropriate feelings of guilt
- Loss of sex drive
- Thoughts about suicide or suicide attempts
Causes
The exact cause of depression is not known, but the likelihood that somebody will decome depressed seems to be determined by a combination of physical, psychological and social factors.
Some types of depression run in families, so it's thought that some people inherit a genetic predisposition for it. In identical twins, if one twin is diagnosed with clinical depression, the other twin has around a 46% chance of developing one too. Other people affected by depression have no family history of mental illness, but they may be vulnerable to depression because they have picked up very negative ways of thinking. Low self-esteem and distorted thinking are closely related to depression, although it's not always clear if they are a cause or an effect.
Depression can be triggered by a traumatic event or period of stress, such as a bereavement, losing a job, family problems, divorce, exam stress, poverty or social isolation. Substance abuse and certain chronic illnesses (e.g. hypothyroidism) also make people more likely to develop depression.
More about depression:
Sources:
1. The Depression Alliance - Now We're Talking (April 17, 2007)
2. NPR - History of Treating Depression (2004)
3. Karl Hempel, M.D. - Depression: What you need to know
Subscribe to:
Comments (Atom)